Corneal Implants: KAMRA, TEARDROP
Intracorneal presbyopia devices like rings work by inducing a pin-hole effect and thus increasing the depth of focus thus allowing for increased near vision. They are implanted in to the cornea stroma and require the use of a femtosecond laser to create an implantation pocket prior to their insertion. Like multifocal lenses, they too induce high order aberrations (HOA) and affect quality of vision (QoV).
BEST CANDIDATES
Individuals over 40 in need of reading glasses
- Procedure time: about 15 minutes per eye
- Typical results: clear vision at all distances without glasses or contact lenses
- Recovery time: several days to several weeks
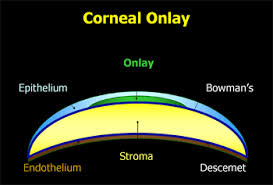
Corneal inlays and corneal onlays are tiny lenses or other optical devices that are inserted into the cornea to improve reading vision. Some of these devices resemble very small contact lens. The primary purpose of these devices is to improve near vision and reduce the need for reading glasses in older adults who have presbyopia.
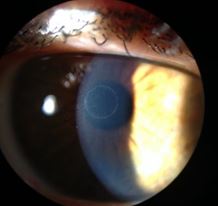
As their names suggest, corneal inlays and onlays differ in where they are implanted within the cornea: corneal onlays are placed near the surface of the eye, directly under the thin outer layer of the cornea called the epithelium; inlays are placed deeper in the cornea — in the thicker middle layer called the stroma.
Corneal inlays are placed within the central stromal layer of the cornea; corneal onlays are positioned just beneath the outer epithelium.
Because they are implanted deeper in the cornea, corneal inlays may be more stable and deliver more predictable and long-lasting results than corneal onlays. For these reasons, it appears corneal inlays will likely be the preferred device for doctors and patients interested in this refractive surgery option.
Corneal inlay surgery sometimes can be combined with LES to correct both presbyopia and shortsightedness, farsightedness and/or astigmatism. This surgery is less invasive and may have fewer risks than phakic IOL or ICL procedures, which involve implanting lenses further back inside the eye either directly behind or in front of the pupil. Also, because no corneal tissue is removed during inlay surgery, this procedure may be a good alternative for people whose corneas are too thin for LASIK or LASEK.
Kamra Corneal Inlay
Developed by AcuFocus, the Kamra corneal inlay received FDA approval for use in the United States in April 2015. The device also has received a CE mark for the European Economic Area, allowing it to be marketed in over 30 countries across Europe.
The Kamra inlay is designed to reduce or eliminate the need for reading glasses among people over age 40 who have good distance vision without glasses but have problems seeing up close due to presbyopia.
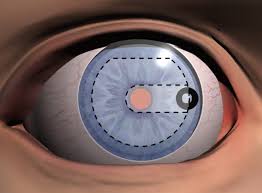
The Kamra device is very small and thin — just 3.8 millimeters (about 0.15 inch) in diameter and 6 microns thick (about half the thickness of plastic wrap foil – clingfilm used to store food). It consists of an opaque outer ring and a tiny (1.6 mm) central opening that is placed directly in front of the center of the pupil. This creates a pinhole camera effect that extends the natural range of vision, making near objects appear clearer without significant loss of distance vision.
The Kamra inlay typically is implanted in the non-dominant eye, so the distance vision of the patient’s dominant eye is completely unaffected. The procedure takes less than 15 minutes and can be performed in the eye surgeon’s office. The eye heals quickly without the need for stitches.
Raindrop Near Vision Inlay
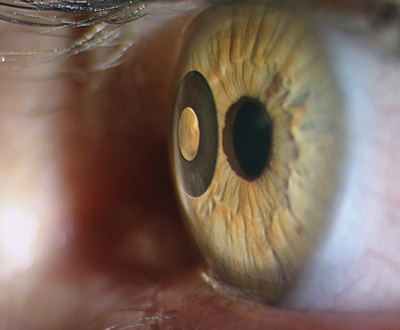
The Raindrop Near Vision Inlay is a corneal inlay for presbyopia being developed by Revision Optics. Formerly known as PresbyLens in the U.S. and Vue+ in Europe, the tiny (2.0 mm diameter) inlay is made of medical-grade hydrogel plastic similar to that used for soft contact lenses and has optical characteristics that are almost identical to the human cornea, according to the company.
The Raindrop Near Vision Inlay typically is placed within the cornea of the non-dominant eye under a LASIK-style flap. When in position, the inlay changes the curvature of the cornea so the front of the eye acts much like a multifocal contact lens.
In a recent study of 38 people (ages 45 to 56) who underwent the Raindrop Near Vision Inlay procedure:
- Six months after receiving the implant, most people could perform near vision tasks such as reading a newspaper without the need for spectacles.
- Most subjects also did not require glasses for intermediate tasks such as reading a computer screen.
- All study participants had 20/25 or better distance vision in both eyes.
- Only one adverse event was reported, when an inlay needed to be repositioned.
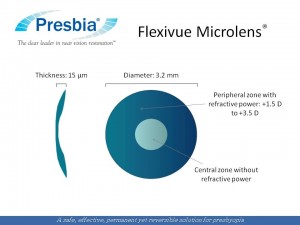
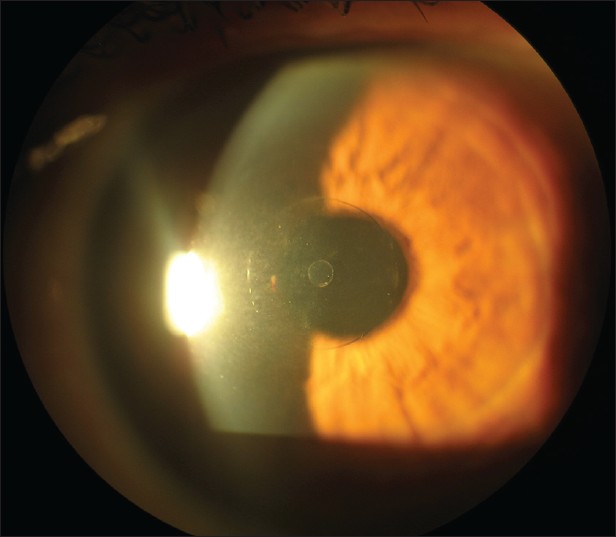
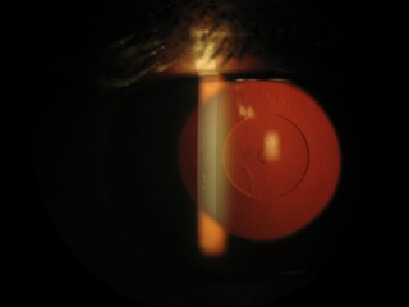
Presbia Flexivue Microlens
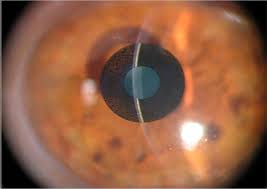
Another innovative corneal inlay designed for the correction of presbyopia is the Presbia Flexivue Microlens, being developed by Ireland-based Presbia PLC. This device resembles a tiny bifocal IOL like those used in cataract surgery. It measures just 3.2 mm in diameter and is available in a range of powers, depending on the patient’s near vision needs.
During the Presbia Flexivue Microlens procedure, small pocket is created in the corneal stroma with a femtosecond laser, and the inlay is inserted into this pocket with a special device. The pocket seals itself, and the entire procedure typically takes less than 10 minutes. The corneal inlay can be removed and replaced with a higher or lower power lens if needed.
In a 2012 study, patients in Italy and Greece who underwent the Flexivue Microlens procedure reported very high satisfaction rates one year after implantation, with 97 percent saying their uncorrected near vision in the implanted eye was either good or excellent, and 97 percent reporting that their uncorrected distance vision with both eyes open was either good or excellent.
Corneal Onlays
Corneal onlays are similar to corneal inlays, but are designed to be placed closer to the front surface of the cornea, just under the outer layer called the epithelium.
The corneal epithelium comprises about 10 percent of the overall thickness of the cornea and acts as a protective barrier to keep bacteria, dust and other foreign substances from penetrating the eye. The epithelium also absorbs oxygen and nutrients from the tear film so they can nourish the rest of the cornea.
Though some research in developing corneal onlays is ongoing in Europe, it appears that corneal inlays have become the preferred technology for corneal implants designed for vision correction
MORE INFORMATION: