This is the basic information I provide in my consultations for an RLE/CLE or cataract procedure with the implantation of a modern multifocal lens. It is important that you read the below as if you were preparing for an examination so that you retain critical information and generate thoughtful questions for our consultation.
Having an elective surgery with a multifocal lens is a very serious decision. Similar to sitting your driving test (and you need to demonstrate basic understanding of traffic laws and driving skill) you need to demonstrate to me your understanding of the risks you are taking because the outcome cannot be demonstrated prior to the surgery and there are no guarantees.
Most of the time patients worry and say ‘I hope it goes well and is successful’. The success of this surgery depends more on your expectations rather than the occurrence or not of any complications. This is 100% successful in that I will remove your natural lens and replace it with an artificial one. The important point is what this new lens can do for you and whether this matches or approximates your expectations. Being a surgery nobody can promise or guarantee anything to you. It will be wrong and unethical to do so.
The choice of a multifocal lens is currently the best possible solution for spectacle independence, however, it is a COMPROMISE (therefore, it is not indicated for perfectionists). Indeed, after surgery, 90% of the patients are able to read the newspaper print under good lighting conditions and 10% of the patients still need to use spectacles for reading or computer work.
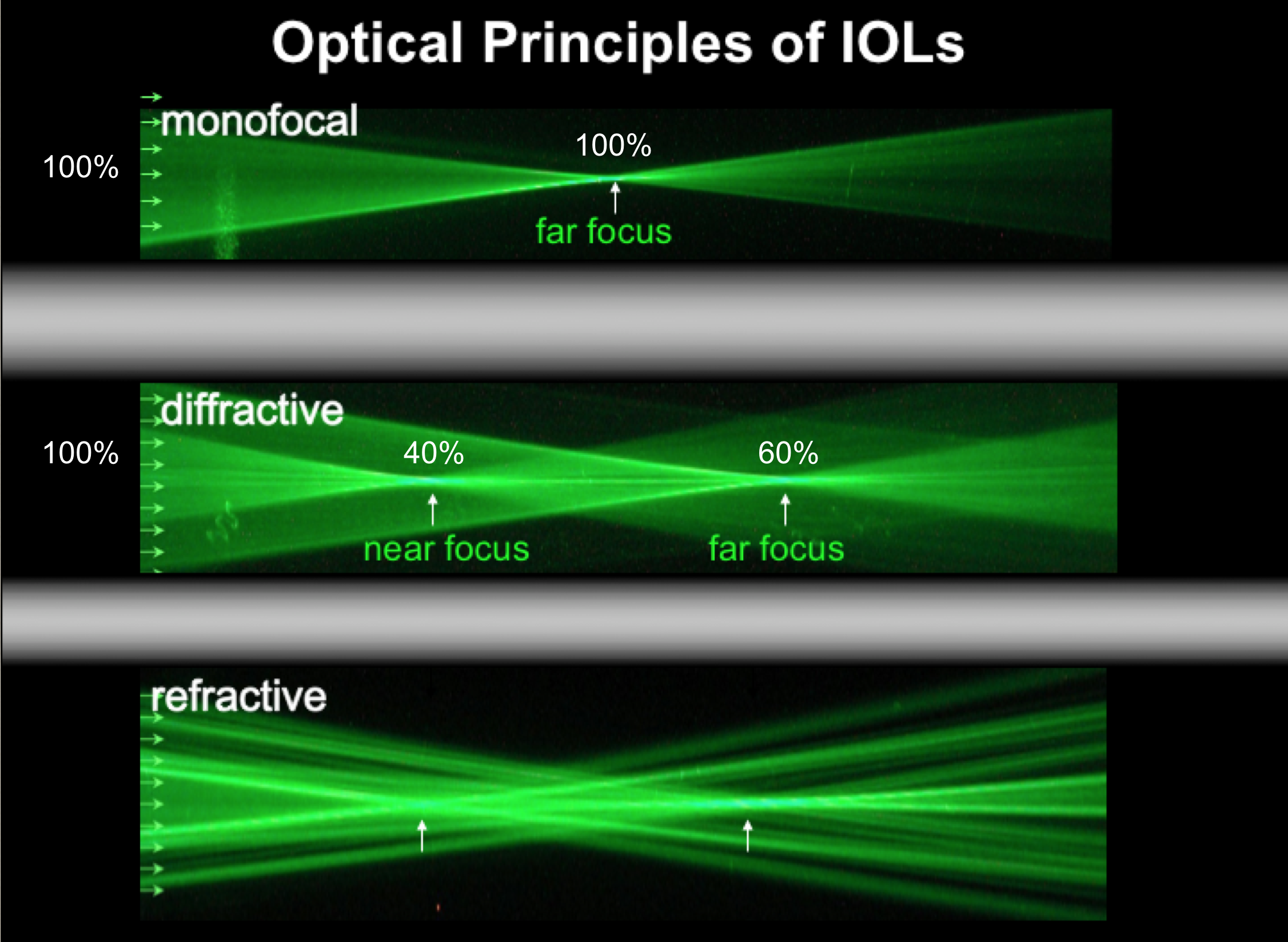
To understand this it is important you appreciate how a multifocal lens work. All through your life, your vision was monofocal and through a process called accommodation (until the age of 40-45) you were able to change the shape of the natural lens inside your eye thus moving the focus from near to distance according to your wish. This is the best possible vision as it utilises all available light (100%), however, technology to do this full lens movement does not exist. The best alternative is a lens with fixed optics that allows for some light to do the near work and the rest to do the distance.
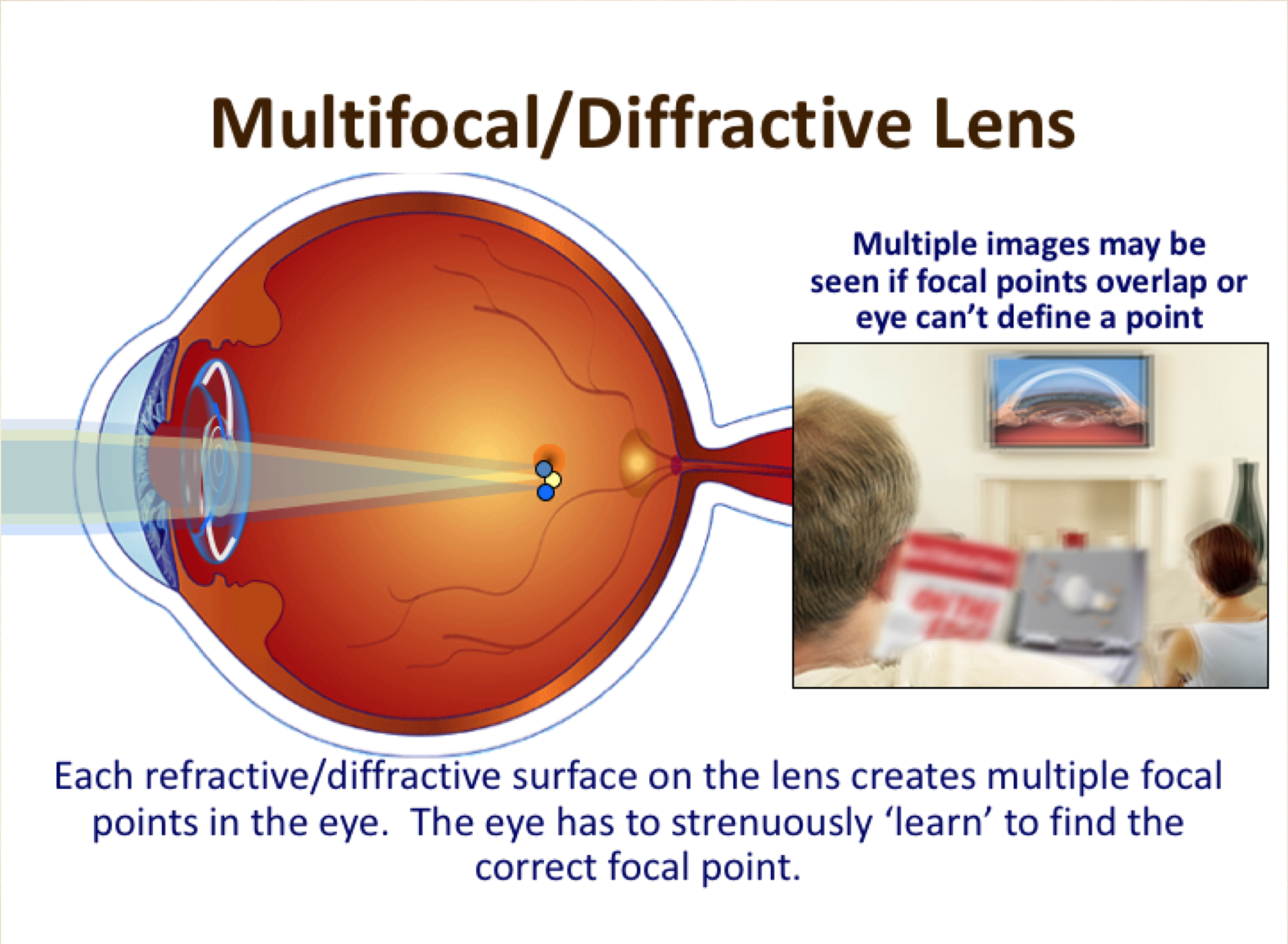 After the surgery, the multifocal lens that will now be sitting behind your pupil will be using 60-80% (depending on lens model) of the amount of light for distance vision and the rest 20-40% for near (reading) and intermediate (computer) vision. Clearly, the stronger the split of light, the better the near vision and the higher risk of blurry, foggy or glary vision. This requires neuroadaptation. This is something the brain can do as is not the eyes but the brain that is responsible for what we make sense in our visual world.
After the surgery, the multifocal lens that will now be sitting behind your pupil will be using 60-80% (depending on lens model) of the amount of light for distance vision and the rest 20-40% for near (reading) and intermediate (computer) vision. Clearly, the stronger the split of light, the better the near vision and the higher risk of blurry, foggy or glary vision. This requires neuroadaptation. This is something the brain can do as is not the eyes but the brain that is responsible for what we make sense in our visual world.
This means that the vision will be a little bit weaker, especially if you are in an environment that the light is not bright enough (as is in the evening and at night). Therefore, do not expect to have as good distance or near vision as you currently do with your respective glasses. In other words, when you assess the result of the surgery a day or a week later (when you will be coming for your 2nd eye surgery) you would be expected to say: ‘yes, I can see well distance and well near, however, my vision is a bit blurry! why?’ The answer is because you’re using only 60% of the light on the treated eye for the distance vision and you are comparing this to the other eye that uses 100% and obviously that cannot be the same unless you have had a cataract.
Side effects and complications
This is also the reason why the two common side-effects (SE’s) of the surgery occur. The glare at night and ghosting happen because when you look in the distance at the headlights of the oncoming traffic or say the subtitles on a movie, the light that passes through the reading part of the lens creates an out-of-focus image (ghost image) that scatters light inside the eye. This is something that the brain will adapt within months without major problems but for less than 1% of the patients, this could mean an inability to drive safely at night for up to a year. Other less prominent SE’s include edge effects, narrowing of the visual field, seeing through a fish ball, floaters, dry eyes.
Overall, when asked a year after the surgery 96% of patients are happy with the outcome of their surgery (that is 85% for plano presbyopes: people that need only reading specs) and recommend it to their friends and relatives despite the fact that 10% of them still use some form of glasses and 5% have some problems with night driving.
The main complications (all can be helped with additional treatment) are:
- Refractive Surprise: 10% of the patients (usually their 1st eye) would require additional laser treatment to correct residual prescription (this would account for more “blurry” than expected vision) this is higher if you had a previous eye surgery (laser or otherwise)
- PCO: 5% per year. An opacification of the bag that surrounds the lens and decreases vision. It is easily treatable with YAG-Laser, a 20 seconds non-invasive cleaning done as an outpatient appointment.
- Iritis: 2 to 5 in 100. Mild inflammation after cessation of drops. Easily treatable with more steroidal drops.
- CME: 1 in 300. It is a bruising of the back of the eye starting around 2 months after surgery, induces blurred vision for a couple of months but settles spontaneously.
- PC Tear with/out Vitreous loss: 1 in 1000. A tear in the bag that contains the natural lens and now will have the artificial lens. This may affect the position or choice of lens implantation (esp. in hard cataracts).
- IOL Exchange: 3 in 1000. This non-routine surgery involves the change of a MF lens to monofocal due to intolerability of SE’s. Surgery takes place 9 -18 months later and results in loss of near vision.
- Retinal Detachment: 1 in 3000. A separation of the retina from the wall of the eye like a wallpaper coming off of the wall. It is more common in shortsighted patients and those under the age of 50.
- Infection: 1 in 10.000. This is the most serious complication and may lead to vision loss depending on the type of microbe involved. It is unlikely to happen after the first few weeks.
Helpful videos from the manufacturers of the intraocular lenses:
- Video of a Tecnis Multifocal IOL: Split of light 60/40% (better near, less distance)
- Video of a Tecnis Symfony EDOF lens: Split of light 80/20% (better distance, less near)





Recent Comments